Public Health Response to the COVID-19 Pandemic in Oregon
-
The purpose of this study is to fulfill the requirements of Senate Bill 1554 (2022), which calls for a comprehensive study of Oregon’s public health system COVID-19 pandemic response. The study aims to comprehensively examine Oregon’s public health system response to the COVID-19 pandemic, identify lessons learned from COVID-19 response, and outline recommendations for improving and strengthening Oregon’s public health system capacity and resiliency for responding to future public health emergencies. Rede Group will submit results of this study to Oregon Health Authority, in three mandated reports in November 2022, March 2023, and September 2023
This study is not an external evaluation of an individual’s, team’s, or agency’s performance, but instead is a systematic examination of Oregon’s complex and evolving public health system response to the COVID-19 pandemic. As such, this study takes into account the perspectives of a diverse array of organizations engaged in the pandemic response across the state. To ensure objectivity, reduce bias, and provide neutrality OHA contracted with Rede Group (based on results of an open, competitive solicitation process) to conduct this study. Rede Group has no affiliation with Oregon's public health system response to the COVID-19 pandemic and was not involved in Oregon's public health system response.
-
Public health is the science of protecting and improving the health of people and their communities (Center for Disease Control and Prevention [CDC], n.d.). Therefore, public health work includes promoting healthy lifestyles, researching disease and injury prevention, and detecting, preventing, and responding to infectious diseases.
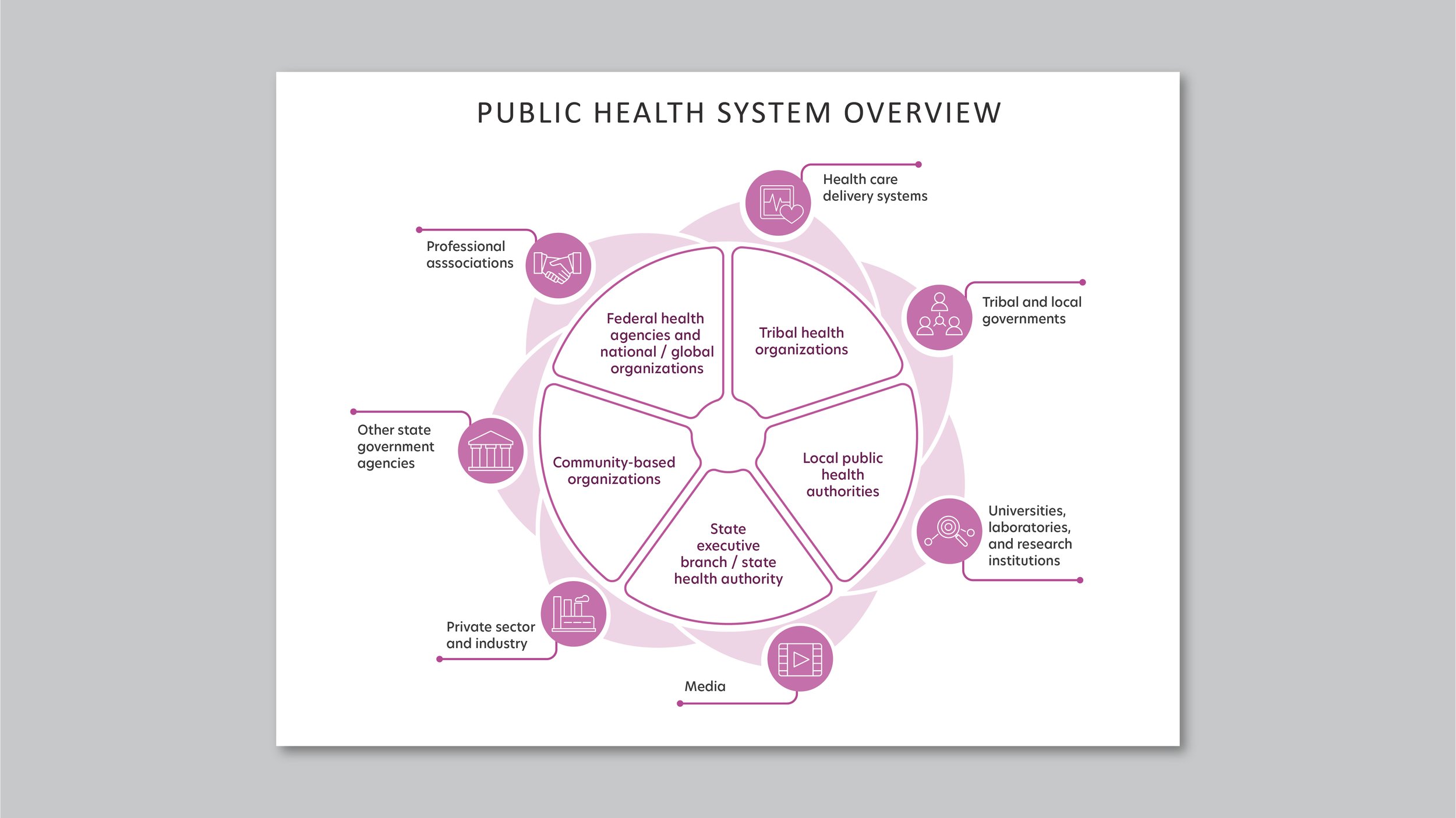
A public health system, typically defined as, “all public, private, and voluntary entities that contribute to the delivery of essential public health services within a jurisdiction”, is formed by a network of actors including government agencies, laboratories, and hospitals, nongovernmental public and private agencies, and community members (CDC, 2021). Public health systems focus on protecting and promoting the health of populations across an array of ecological levels, including community-, state-, national-, and global-levels. Regardless of scale, a well-functioning public health system requires aligned goals, clarity about the distinct roles of each actor, a strong infrastructure that supports coordination and collaboration, and sufficient resources to accomplish its mission.
National standards for public health were initially released by the Centers for Disease Control and Prevention (CDC) in 1994 and updated in 2020 (CDC, 2021). The CDC outlines 10 essential public health services, spanning assessment and monitoring, investigation, communication, community partnership, program and policy implementation, regulation, equitable access to care, workforce development, evaluation and continuous quality improvement, and infrastructure. In 2015, the Oregon Legislature passed House Bill 3100, which aimed to improve the efficiency and effectiveness of Oregon’s public health system through establishing a framework of 11 foundational capabilities and programs. In turn, HB 3100 launched an effort to modernize the public health system with focused investments on identified gaps in the foundational capabilities and programs.
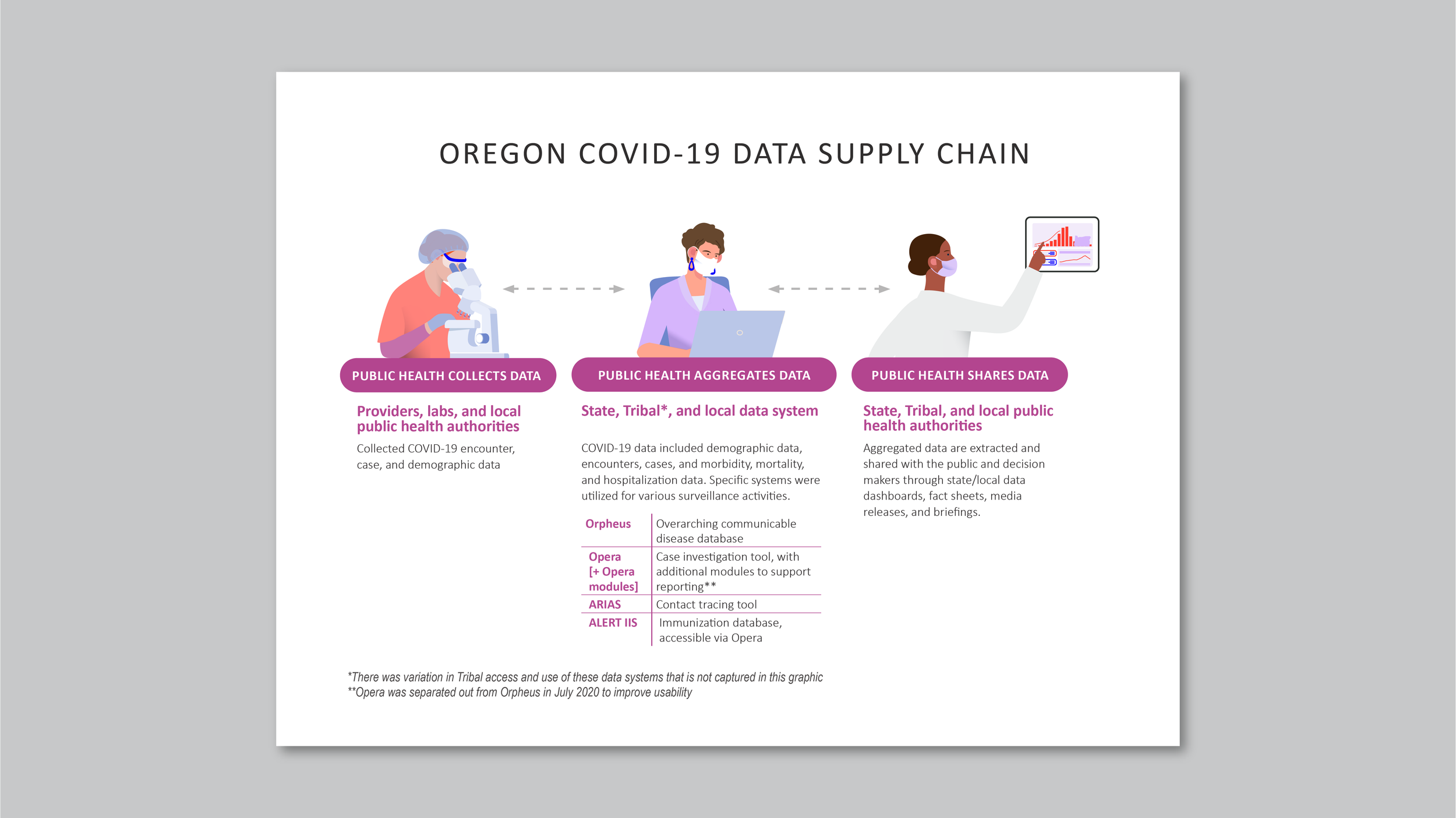
Embedded within Oregon’s public health system is a network of diverse partners composed of state, local, and Tribal agencies, health care delivery partners, private organizations, universities, professional associations, and other partners. For more than two years, Oregon’s public health system has been responding to the COVID-19 pandemic, with each of these partners playing a critical role in the delivery of essential public health services. Whether messaging public health guidance for communities, contact tracing, providing essential goods for individuals during quarantine and isolation, delivering vaccines, or other critical public health pandemic response activities, the importance of each actor’s role and the coordination of efforts within communities and across the state is essential.
Pursuant to Senate Bill 1554 (2022), this study covers Oregon’s public health system response to COVID-19 from the beginning of the pandemic (March 2020) to July 2022. Although Oregon’s public health response to COVID-19 during 2020 -2022 included numerous entities and individuals, this study primarily focuses on governmental public health agencies and other organizations, such as community-based organizations, funded by the governmental public health system to support pandemic response. These entities included federal health agencies and national/global organizations, state executive branch/state health authority, Tribal health organizations, local public health authorities, and community-based organizations. Importantly, Oregon’s health care system, social service sector, higher education system, industries, and businesses were all represented in Oregon’s public health system response to the COVID-19 pandemic. These partners, however, are beyond the scope of this study.
-
In December 2019, the novel coronavirus disease (COVID-19), caused by the SARS-CoV-2 virus, emerged from Wuhan, China and began spreading rapidly throughout China and across the globe. Over the last two and a half years (2020-2022), the COVID-19 pandemic has ravaged health care and public health systems, delivered lasting blows to the global economy, and forever changed the lives of individuals and communities. The global toll of the COVID-19 pandemic has been catastrophic, with 6,524,568 total COVID-19 deaths and 615,310,890 confirmed cases as of September 30, 2022 (World Health Organization [WHO], n.d.). Since the initial outbreak, the public health and emergency response communities have mobilized to research, report, and track the disease, implement evidence-based public health measures that prevent and mitigate widespread transmission, and attempted to resource communities to address the long-term health, social, and economic impacts of COVID-19.
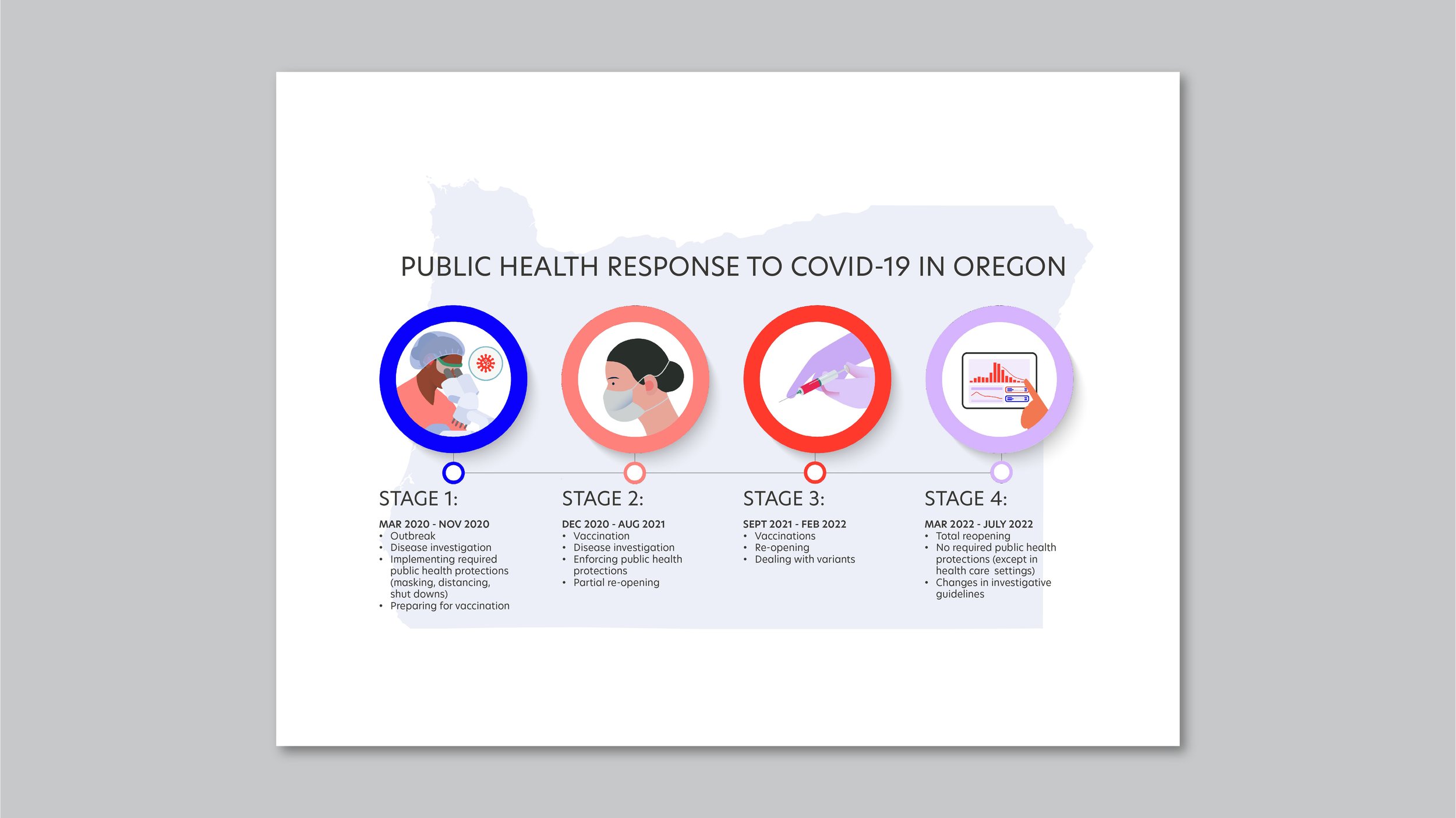
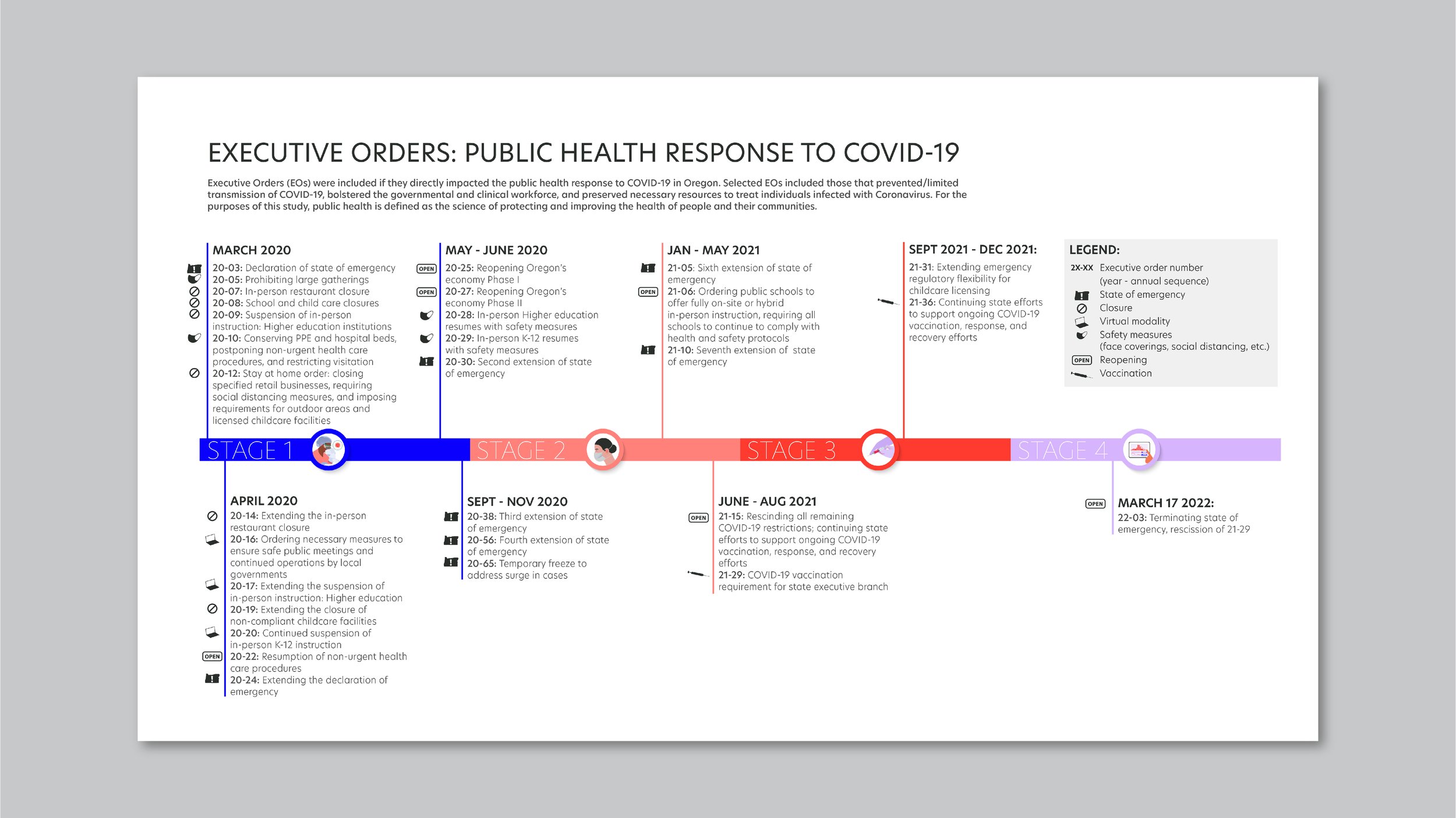
Oregon’s first case of COVID-19 was identified on February 28, 2020 and confirmed March 1, 2020. Though the latest research now indicates that COVID-19 was likely circulating in Oregon and across the U.S. as early as December 2019, widespread transmission and public awareness grew rapidly beginning in March 2020 (Basavaraju et al, 2020). At that time, Governor Kate Brown issued Executive Order 20-03, which declared a state of emergency in Oregon and authorized action to respond to, control, mitigate, and recover from the emergency. Between March 2020 and July 2022 Governor Brown issued 39 executive orders to control the spread of the virus and protect the public’s health.
The pandemic progressed in multiple waves with COVID-19 cases surging and declining due to a variety of environmental factors as well as the evolution of the coronavirus itself. New information about the disease emerged and informed the mounting public health response. Evidence-based public health practices that Oregon implemented to help control the pandemic included public information campaigns, gathering bans, stay-at-home orders, restaurant and bar closures, school and workplace closures, mask mandates, and vaccine mandates, among others. Waves of federal and state emergency response and recovery funding supported Oregon’s public health system response as well. Despite these efforts, the impact of COVID-19 in Oregon has still been great, with 8,561 total deaths and 894,776 confirmed cases as of September 28, 2022 (Oregon Health Authority [OHA], n.d.).
One critical aspect of studying Oregon’s public health response to COVID-19 is acknowledging that the burden of the pandemic was not experienced equally. The population health impacts of COVID-19 have cast light on longstanding inequities in access to health care, educational and economic opportunity, and safety. Racism, ableism, sexual orientation and gender identity discrimination, and other systemic biases have persistently undermined the physical, social, economic, and emotional health of entire communities and populations across Oregon and the nation long before the COVID-19 pandemic. Attention must be given to understanding the disparities in COVID-19 outcomes and intentionally addressing the root causes of inequities throughout the long-term COVID-19 public health response and recovery.